Biomedical Engineers Develop Nanoparticles to Fight Persistent Viral Infections
Many sexually transmitted diseases spread by bacteria, like syphilis and chlamydia, can be controlled and cured with antibiotics. By comparison, cheap and effective treatments for viral STDs have largely remained elusive. Researchers in Mark Saltzman’s lab are working to change that, developing nanoparticles to prevent infection by a widespread viral STD: herpes simplex virus type 2.
HSV-2 is unfortunately common in the United States. About one of every six people between the ages of 14 and 49 years has a genital herpes infection, and while the infection can be managed with treatment, it can’t be cured. Worse, HSV-2 leaves individuals more vulnerable to additional infections, including HIV.
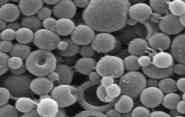
Saltzman, the Goizueta Foundation Professor of Biomedical Engineering, Chemical & Environmental Engineering & Physiology, has developed nanoparticles that deliver molecules to the potential infection site with the hope of preventing and treating HSV-2 infection.
In a paper in the Journal of Controlled Release, Saltzman and colleagues demonstrate that topical administration of their nanoparticles can improve survival after HSV-2 infection in mice. The nanoparticles carry short interfering RNA (siRNA) molecules that have been shown to interfere with nectin-1, a protein involved in HSV-2 infection and cell-to-cell transmission. In their experiments, the researchers showed that their nanoparticles can both prevent lethal infection with HSV-2 in mice and increase survival time when administered in 3 applications, before and after infection.
“This work provides proof-of-concept that these siRNA delivery vehicles are promising options for topical, localized therapeutics for sexually transmitted infections,” says Jill Steinbach, a postdoctoral researcher in Saltzman’s group and the lead author of the paper. “We are excited to see such encouraging results of decreased symptoms associated with infection, and enhanced survival out to an unprecedented duration of 28 days.”
Critically, the nanoparticles also improved survival time without causing inflammation at the administration site, which can leave patients vulnerable to additional infections and has been a problem with previous experimental efforts.
Further, the researchers’ nanoparticles, made from polylactic-co-glycolic acid (PLGA), use materials that have already been approved by the FDA, which could facilitate faster approval of treatments for humans down the road, whether they are to be used against HSV-2 or additional pathogens.
“We are encouraged in the potential of these tunable PLGA nanoparticles to provide a safe, durable, and non-toxic alternative to other microbicides that have been shown to promote infection through inflammation of the intravaginal tract,” says Steinbach. “Currently, we seek to enhance nanoparticle delivery by using a variety of surface modifications that enable increased cell penetration, while obtaining a better understanding of how the delivery vehicles interact with the cell to exert their effect. We are hopeful to further improve delivery of these materials and apply them to a wide range of pathologies in global health.”